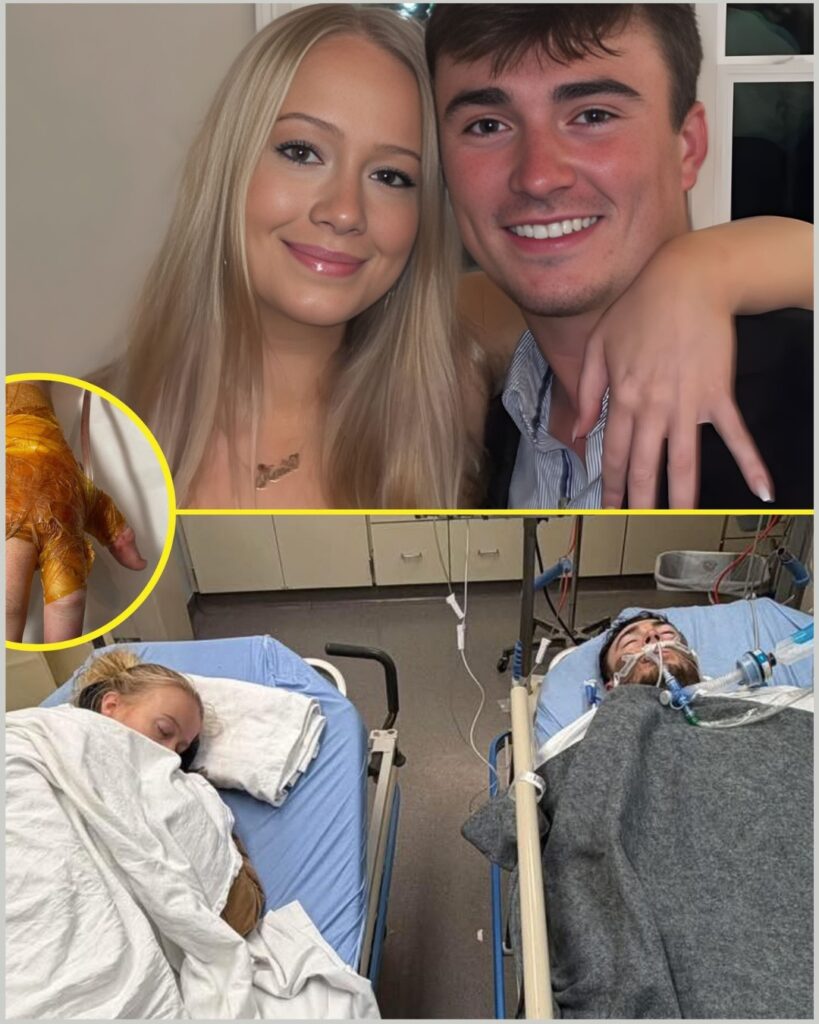
d+ She Hasn’t Left the ICU: Inside the Long Nights Before Hunter’s Next High-Risk Surgery
The lights in the intensive care unit never fully dim. Even at 3 a.m., the room glows in soft blues and steady green pulses, the rhythm of machines filling the silence that no one dares to break. In the corner, curled into a rigid hospital chair, Katie keeps watch.
She hasn’t gone home.
She hasn’t slept in her own bed.
For days now, the ICU has become her address — not because anyone required it, but because she chose it. Because Hunter is here. And right now, that is the only place she believes she should be.
As Hunter prepares for another major operation, the atmosphere inside his hospital room has shifted. Doctors move in and out more frequently. Conversations happen just outside the curtain, voices lowered, sentences careful. Words like “risk,” “complication,” and “stability” drift through the air, landing heavier than they did before his last procedure.
This time feels different.
Hunter’s injuries — severe trauma to both arms — have already required intense intervention. He is awake now, able to move lightly within strict medical limits. But recovery has not followed a straight line. There have been setbacks, concerns, and the kind of medical decisions that require weighing hope against probability.
And so the next operation looms.
“It’s not routine,” one member of the care team acknowledged quietly. “We’re proceeding carefully.”
That carefulness is what keeps Katie rooted in place.
She sits close enough to hear every change in the monitor’s rhythm. Close enough to feel the warmth of Hunter’s hand in hers. When nurses adjust dressings or check vitals, she stands but never steps far. When specialists gather around imaging scans, she watches their faces as much as the screens.
The exhaustion shows. There are faint shadows beneath her eyes. Her posture stiffens after hours without movement. But leaving, even briefly, feels unthinkable.
“Time moves differently in here,” a nurse explained. “For families, especially. Every minute stretches.”
Katie knows that stretch intimately now. Days blend together — morning rounds, medication schedules, the soft shuffle of rubber soles on polished floors. Meals arrive untouched until someone reminds her to eat. The outside world feels distant, almost abstract. What matters is the steady rise and fall of Hunter’s chest and the data streaming across the monitors above him.
In a space defined by uncertainty, she has become the one constant.
It is a role she did not anticipate but has stepped into fully — advocate, observer, emotional anchor. She listens closely when surgeons outline the plan for the upcoming operation. She asks questions when terminology becomes dense. She absorbs the warnings that precede consent forms.
The doctors have been transparent: this next procedure carries more pressure than the last.
Scar tissue complicates access. Previous trauma increases sensitivity. The margin for error narrows with each intervention. While optimism remains, so does realism. It is a balance the medical team walks carefully — offering reassurance without minimizing risk.
For Katie, those conversations are the hardest part.
One physician, according to a source familiar with the discussion, took a moment before the latest briefing to prepare her. Complications, though unlikely, cannot be ruled out. Recovery may be slower this time. Pain management could be more complex. There are scenarios that must be discussed, even if no one wants to imagine them unfolding.
She listened without interrupting.
Later, back in the ICU room, there was a quiet moment that seemed to shake her more than the medical terminology had. Hunter shifted slightly, wincing, and asked a simple question about how much longer it would take to “feel normal again.”
Katie paused before answering.
Because normal, at least for now, is undefined.
The emotional weight of this stage of recovery is becoming harder to disguise. The first surgery carried urgency — a race against time. This one carries expectation. There is more to lose. More to protect. More history behind them.
“It becomes about endurance,” another staff member noted. “Not just physical endurance, but emotional.”
Endurance is visible in the way Katie steadies her voice when Hunter’s frustration surfaces. In the way she smooths the hospital blanket without thinking. In the way she refuses to let fear dictate her tone, even when it presses in from every direction.
She has become fluent in the language of beeps and charts. She knows which alarms require immediate concern and which signal routine adjustments. She anticipates shift changes. She recognizes the subtle expressions on doctors’ faces — the almost imperceptible relief when numbers improve, the thoughtful silence when they don’t.
Outside the ICU, life continues. Messages accumulate on her phone. Support pours in from friends and community members who follow each update closely. But inside the room, everything narrows to one purpose: getting Hunter through the next step.
The upcoming operation has no guarantee attached to it. No promise of instant resolution. Only the possibility of progress — and the understanding that progress, in cases like this, often arrives inch by inch.
As surgery approaches, preparations intensify. Pre-operative evaluations. Adjustments to medication. Final imaging reviews. The clinical choreography unfolds with precision, but emotion remains unpredictable.
When the time comes to wheel Hunter toward the operating room again, Katie will likely walk beside the gurney until hospital policy requires her to stop. She will watch the doors close, just as she did before, and measure time in heartbeats rather than minutes.
For now, she remains in the chair.
Holding his hand.
Watching every monitor.
Refusing to miss a single moment that could matter.
In the controlled chaos of intensive care, where uncertainty is a constant companion, love has taken on a quiet, stubborn form. It looks like sleepless nights. Like whispered encouragement. Like choosing a cold hospital chair over comfort because leaving feels like surrender.
This story is no longer only about surgery. It is about how long someone can stand upright when fear surrounds them. It is about resilience measured not in dramatic gestures, but in presence.
As Hunter moves closer to the operating room once more, the tension in the ICU thickens. The machines continue their steady hum. The staff prepares with practiced focus.
And Katie stays.
Because sometimes, in a fight that refuses to slow down, being there — fully, unwaveringly there — is the only thing that feels within her control.

